When faced with the death of a family member, you may endure a roller coaster of emotions. Having the proper people around you can make a huge difference in your capacity to love and support your loved one. A nurse's role in end-of-life care often entails giving comfort and symptom treatment.
Palliative Care
Palliative care is largely supportive care for persons with life-threatening illnesses, with the goal of improving the patient's quality of life while undergoing treatment. It encompasses all other end-of-life care therapies, including as pain and other physical symptom management, support for the patient's family and friends, physical care such as eating, dressing, and bathing, and emotional support for the patients.
It should be highlighted that obtaining palliative care does not necessarily imply that one's life is coming to an end. Palliative care is sometimes required for patients undergoing treatments such as radiotherapy or chemotherapy. Palliative care can be used in conjunction with other medications and therapies.
Palliative Care Advantages
Palliative care relieves disease-related symptoms such as pain, persistent fatigue, and muscle weakness. It can also assist to alleviate emotional symptoms like depression and anxiety.
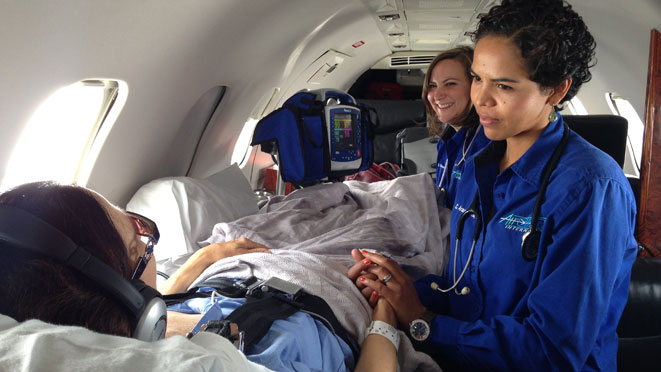
Palliative care nurses use an integrative and multidisciplinary therapy strategy to assist patients in maintaining their physical, mental, and emotional health.
They take the time to understand each patient's needs in order to develop a personalized treatment plan that gives long-term comfort.
Palliative care plays an important part in the long-term care of you or a loved one by stressing the improvement of a patient's quality of life.
Preparing for Long-Term Care
Advance directives represent the values of a patient. When someone is unable or unwilling to speak, advance instructions are employed. A surrogate represents the patient's desires in advance directives. MOLST is an advance directive (medical orders for life-sustaining treatment). Oral communication with a family member or health care practitioner may also be beneficial. Pre-advance directives should represent discussions and decisions made while the patient is still alive. It is recommended that advance directives be created with the patient's family and doctor.
Coordination of Care
All of the dying person's care and treatment needs, as well as their wishes, are conveyed to everyone who comes into contact with them. If feasible, one person takes responsibility for this, who may or may not be a nurse. That individual ensures that the chosen deputy is available to the dying person, their family, and other care providers in order to ensure that the plan of care is implemented. This can help reduce stress and tension in these challenging times.
End-of-life nursing covers several areas of care, including pain and symptom management, culturally sensitive approaches, guiding patients and families through the death and dying process, and making ethical decisions. The typical time frame for persons receiving end-of-life care is difficult to estimate, and while many people associate end-of-life care with death, some patients may receive end-of-life care for many years. Nurses serve as advocates, ensuring that the patient's and family's final wishes are carried out.
Download the app for easier use